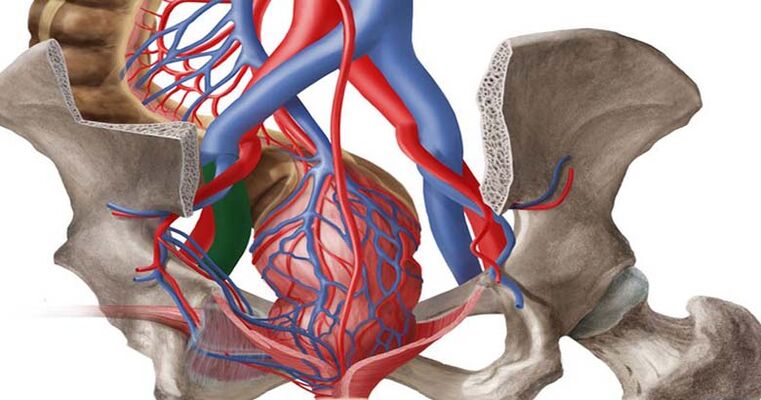
What are minor pelvic varicose veins?
Classification of small pelvic varicose veins
Small pelvic varicose veins
- Vaginal and external genital (perineal) varicose veins- Characterized by structural changes in the large ductus venosus affecting the external genital veins. The cause is usually a long pregnancy, during which the enlarging uterus compresses the inferior vena cava and iliac veins.
- venous congestion syndrome- Characterized by the dilation and stretching of the veins in the small pelvis and the backflow of blood through them. The causes of this reflux can vary.
Stages of minor pelvic varicose veins
- The first stage
It is characterized by dilated veins up to 5 mm in diameter. Blood vessel tone is reduced and the network takes on a tortuous appearance. - second stage
It is characterized by decreased elasticity of the pelvic vascular bed. The dilated veins are 6 to 10 mm in diameter. The parametrial vessels and ovarian plexus are affected. - The third phase
It is characterized by complete damage to vascular fibers. Expanded diameter exceeds 10 mm. Against the background of progressive varicose veins, women may develop complications.
development nature
- Primary varicose veins in female pelvic veins
It develops in the context of acquired or congenital valvular pathology. Doctors usually talk about venous valvular insufficiency, with the appearance of tortuosity and overstretching of blood vessels. Typically, primary varicose veins are caused by increased physical activity, complications during pregnancy and childbirth, and the use of hormonal medications. - Female pelvic vein secondary varicose veins
is formed in the context of past illness. Infectious diseases, tumors, pelvic endometriosis, and developmental abnormalities of the pelvic organs can all affect the tone of the veins.
Causes of small pelvic varicose veins
- genetics. Often, venous disease in women is hereditary. If a mother, grandmother or aunt in the family has varicose veins, the disease is likely to affect the next generation of women.
- Pelvic organ connective tissue dysplasia. It is a congenital anomaly characterized by reduced collagen production and decreased tone of the blood vessel pattern.
- Pregnant. During pregnancy, the load on muscles and blood vessels increases significantly. The growing uterus puts pressure on adjacent tissues and adjacent veins. Women with polyhydramnios, multiple pregnancies, large fetuses, and other conditions may develop varicose veins.
- Overweight. Obesity in women increases pressure on pelvic organs. Not only can this lead to varicose veins, but it can also lead to other health problems.
- reduced physical activity. The human body requires regular physical activity. We're not talking about a grueling workout. Conversely, excessive physical activity can be an independent cause of small pelvic varicose veins. A sedentary lifestyle disrupts blood flow in the pelvis and a stagnation process occurs.
- hormone imbalance. The entire female body works entirely under the influence of hormonal levels. Hormonal changes and taking hormonal medications may cause a decrease in vascular tone.
Varicose veins of the lower extremities are often accompanied by varicose veins of the small pelvis. If a woman has tortuous blood vessels in her legs, she must undergo a pelvic vascular examination and receive treatment if necessary.
risk factors
- bad habits;
- Overeating;
- Gastrointestinal disruption and tendency to constipation;
- Lack of intimacy;
- difficulty conceiving;
- surgical intervention;
- Pelvic organ damage;
- hormonal treatment;
- Vigorous physical activity.
Symptoms of pelvic varicose veins
- lower abdominal pain;
- Breakthrough abnormal uterine bleeding;
- Discharge not related to the menstrual cycle;
- Feeling of swelling and foreign body in the pelvis;
- Low back pain in sacrum, lower back, legs, perineum;
- Bright PMS;
- Severe pain during menstrual bleeding;
- Discomfort and pain during intimacy;
- Frequent urination;
- Digestive tract dysfunction.
A characteristic feature of female pelvic varicose veins is the formation of tortuous blue veins in the external genital area and vagina.
Diagnosis of pelvic varicose veins
- Visual inspection of external genitalia;
- Check the vagina and cervix with a speculum;
- Palpation and diagnosis of valve function in the inguinal region;
- Ultrasound examination of pelvic organs;
- Doppler studies;
- CT scan;
- magnetic tomography;
- hysteroscopy;
- Laparoscopy.
Treatment of small pelvic varicose veins
Medical treatment of small pelvic varicose veins
- intravenous refills. Modern pharmacology offers many types of intravenous agents. The main task of the drug is to increase the elasticity of blood vessels, normalize blood flow, and stabilize the function of the valves. These medications can be taken internally or in ointment form.
- anticoagulant. These medications are used to treat thickening of the blood caused by pelvic varicose veins. This parameter is determined by laboratory testing. Blood thinners prevent blood clots from forming and reduce blood thickness.
- NSAIDs. Medications are used to treat severe pain and as an additional treatment for the inflammatory process. In general, NSAIDs have symptomatic effects. They can relieve the symptoms of small pelvic varicose veins, but they do not completely solve the problem.
- Vitamin complexes and trace elements. Since most people are nutrient deficient and do not get enough nutrients from food, supplementing their vitamin intake is recommended. For varicose veins, it is recommended to take vitamins B, C, and D.
Surgery
Endovascular embolization can resolve 95% of minor pelvic varicose veins. Going forward, women are advised to engage in lifelong prevention of vascular disease.
General advice for women with pelvic varicose veins
Why are pelvic varicose veins dangerous for women?
- Thromboembolism;
- Thrombophlebitis;
- Venous thrombosis;
- hemorrhoid;
- hormonal imbalance;
- abnormal uterine bleeding;
- chronic pelvic pain;
- Infertility.
Pregnancy and minor pelvic varicose veins
Prevent small pelvic varicose veins
- healthy lifestyle;
- good nutrition;
- Prevent obesity;
- Say no to bad habits;
- moderate physical activity;
- drink enough fluids;
- Refuse to wear high heels for long periods of time;
- Proper pregnancy planning and prevention of pregnancy complications;
- Use compression garments with a higher risk of varicose veins;
- Schedule regular physical exams.


















